Covid Antigen Test Pricing
A COVID-19 antigen test looks for pieces of proteins from the surface of the SARS CoV-2 virus to determine if the person has an active infection. It is faster and less expensive than the molecular or PCR test, but the latter is more accurate.
How much does an antigen test for COVID-19 cost? That depends.
The decentralized healthcare system in the United States leads to wide differences in medical expenses. In the US, the cost and access to antigen testing varies considerably. The price of a COVID-19 antigen test depends on the region of the country, the type of laboratory where the test is processed, the insurance provider, the ultimate payer, and other factors.
The actual cost of an antigen test is estimated to be between $5 to $50. The federal Families First Coronavirus Response Act (FFCRA) currently ensures access to testing for COVID-19 that is free to the patient regardless of insurance status, and prohibits co-pays and deductibles for the test. These CARES Act coverage and payment requirements apply during the duration of the public health emergency.
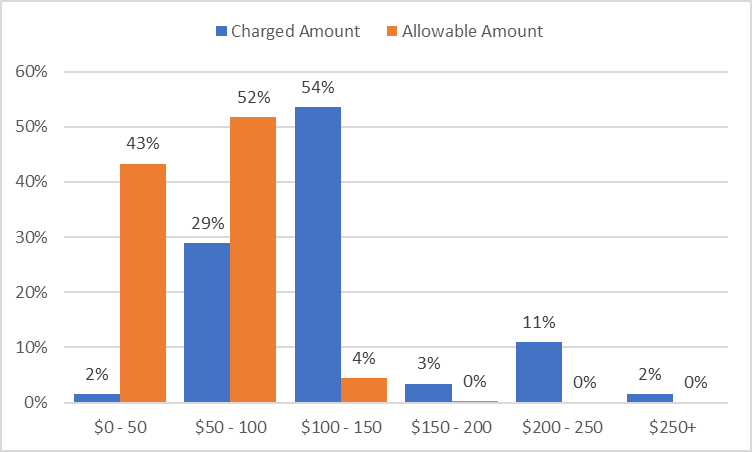
This graph shows the average charged amounts and allowable amounts for COVID-19 antigen tests across the United States. This price data comes from TK Software, a medical claims clearinghouse. This price data reflects the prices for the antigen test only and is specifically for Procedure Code 87426: SARS COV Coronavirus AG IA.
As for other health services, hospitals and laboratories can set their own rates for privately insured and uninsured individuals. Private health insurers then negotiate allowed charges with hospitals and other testing facilities participating in their network. Insurers pay the “Allowable Amount”, the amount actually paid for the test, after negotiating volume or other discounts. If they haven’t negotiated a rate for out-of-network providers, insurers must pay the provider’s cash price–sometimes called the list price–for COVID-19 testing and related services.
There is a wide disparity in charges. The statewide average allowable amount ranges from $19.87 in Rhode Island to $96.00 in California. (It’s $0 in Massachusetts due to state reimbursement.) The mean allowable amount nationwide is $56.41; the median is $55. There is considerable variation within each state, too; the average maximum among the states is $750.
However, the Medicare Administrative Contractor (MAC) price guideline for this same procedure code is only $35.33 for most states, and $45.23 for 12 states, DC, Puerto Rico and the Virgin Islands. In most cases the allowable amounts paid for COVID-19 tests are significantly higher than the amount Medicare allows. Outside of the Medicare program, there is no federal regulation of the price of COVID-19 diagnostic tests or other related tests and visits.
Some testing sites that provide rapid tests are charging hundreds of dollars. Omaha-based GS Labs, which has done over 500,000 tests since the start of the pandemic, regularly bills $380 for COVID-19 tests. Many health insurers consider those charges price gouging, and some refuse to pay those fees.
Availability of free testing sites
There was a marked transition from mass testing sites to mass vaccination sites in 2021. Testing is still generally available through federally qualified health centers, public health clinics and primary care offices. Since January 2022, there has been a rebound in the number of free testing sites across the country, as well as millions of test kits sent to schools.
The price of over-the-counter rapid tests
Over-the-counter rapid antigen tests, while lower-priced than the bills some patients have received from clinics or hospitals, are also overpriced, according to many experts.
Rapid antigen COVID-19 tests can cost around $15 or even as low as $24 for a set of two at pharmacies or supermarkets, if you can find them. In many areas, they haven’t been readily available. They’re still too expensive, given how inexpensive they are to produce and how much is being subsidized by taxpayers through the Defense Production Act, said Jorge Caballero, a San Francisco doctor who co-founded Coders Against COVID, a volunteer group that created a database of COVID-19 testing sites.
In September, President Joe Biden announced that large retailers would sell rapid at-home tests at up to a 35% discount for three months, and that Medicaid would cover the tests for free. Caballero still objects to that amount. “There’s no reason, absolutely no reason, two of these tests should cost any more than $1 to $3,” he said.
Since 15 January 2022, private health insurance companies have been required to cover the costs of up to eight rapid home tests. The Biden administration said it would buy a billion free tests, which people could request online or at local health clinics and pharmacies, for the 28 million Americans without health insurance. It is not clear how many tests have been distributed.
Globally, the costs tend to be far less, or free of charge to the end consumer. Tests cost $3.50 in India and under $1 in Germany. The first 14 tests in the U.K. are free. Canada also gives out free tests to businesses. Of course, in all countries, the taxpayer is picking up the tab.
When “free” is not free: Related costs.
Federal law (the FFCRA) requires insurers to cover the costs of the actual COVID-19 tests, but patients are still being charged for related expenses. These can include up to seven other steps which the law does not require insurers to cover:
- initial COVID-19 screening; this may refer to questioning and measuring of temperature by a health care worker
- an in-person physician’s visit or consultation by telemedicine that may be required before a test will be administered
- a doctor’s referral that may be required before a test will be administered
- a facility fee
- specimen collection
- interpretation of test results
- other diagnostic tests or procedures ordered to confirm COVID-19 or rule out other possible conditions.
Any test would likely require one or more of these additional charges, which could potentially add significantly to the cost.
Opaque pricing or coverage
The prices for medical care have been notoriously opaque in the U.S. Both insured and uninsured patients often find out the full cost only after they receive bills for their care. Hospitals and insurers may keep their negotiated rates secret, allowing the same provider to charge different rates for the same service. Prices for both the COVID-19 antigen test itself and for related expenses can be high and unpredictable.
The CARES Act requires providers to post the cash price for COVID-19 tests on their public websites for insurer use. But in most cases, the total cost of care for a test and its related services is not easy to determine from hospital websites. The charges for COVID-19 testing and related services may be in a bundle, or the patient may receive separate bills from the hospital or testing facility, the attending health professional, the laboratory, and other providers involved in care, which may make it hard to identify or categorize prices.
For instance, the list price for specimen collection ranges from $18-$240. One hospital listed three different charges based on where the specimen was collected–in a skilled nursing facility, at home, or in an outpatient setting. In 2020, one hospital’s price estimator tool demonstrated that the price of COVID-19 screening would be $77 before discounts, and $31 after applying a 60% discount for qualifying self-pay individuals.
Federal law only requires reimbursement for “medically appropriate” testing. An insurance provider might rule that certain reasons for testing (testing after a trip, or if an employer requires frequent testing) may not be considered “medically appropriate.” Furthermore, federal rules don’t apply to certain private plans, such as short-term health insurance policies. For an out-of-network COVID-19 test, private plans are supposed to pay the full price on a provider’s website, but federal law does not stipulate the rules if no cash price is listed.
While the FFCRA and the CARES Act attempted to reduce COVID-19 testing costs for consumers, the cost and growing volume of testing could increase the overall cost of insurance.